Diagnosis

Cirrhosis often is an indolent disease with most patients remaining asymptomatic until the occurrence of decompensation, which is typically characterized by ascites, spontaneous bacterial peritonitis, hepatic encephalopathy or variceal bleeding from portal hypertension. Physical examination of patients with cirrhosis may reveal a number of findings that necessitate a hepatic- or gastrointestinal-based work-up to determine the aetiology. Some patients already may have had laboratory or radiographic tests that incidentally uncovered signs of cirrhosis and its comorbidities. Unfortunately, no serologic or radiographic test can accurately diagnose cirrhosis. Furthermore, a significant correlation occurs between persistently elevated liver function tests and biopsy-proven underlying hepatic disease, and so a more targeted serologic work-up is indicated in patients whose liver function test results are persistently abnormal.
Diagnosing liver cirrhosis1
The single best test for diagnosing cirrhosis is biopsy of the liver. However, as liver biopsies carry a small risk for serious complications, biopsy often is reserved for those patients in whom the diagnosis of the type of liver disease or the presence of cirrhosis is not clear. The possibility of cirrhosis may therefore be suggested by the patient’s history, physical examination or by routine testing. If cirrhosis is present, other tests can be used to determine the severity of the cirrhosis and the presence of complications. Tests also may be used to diagnose the underlying disease that is causing the cirrhosis.
Healthcare professionals should inquire about medical history and risk factors such as:
- Quantity and duration of alcohol consumption
- History or transmission risk for hepatitis B and C
- Family history of autoimmune or hepatic diseases
- Obesity, diabetes, hypertriglyceridemia, profound weight loss after jejunoileal bypass (risk factors of NAFLD, formerly known as non-alcoholic steatohepatitis, NASH)
- A physical examination should also be performed (excluding other causes of signs and symptoms).
- The lower edge of an enlarged liver can be palpated below the right rib cage and feel the tip of the enlarged spleen below the left rib cage. A cirrhotic liver feels firmer and more irregular than a normal liver.
- Some patients with cirrhosis, particularly alcoholic cirrhosis, have telangiectasias on the skin, particularly on the chest.
- Jaundice is common among patients with cirrhosis.
- Ascites and/or edema of the lower extremities due to fluid retention is common among patients with cirrhosis.
- Esophageal varices may be found unexpectedly during upper endoscopy and are strongly suggestive of cirrhosis.
- Reduced levels of albumin in the blood or abnormal bleeding suggest (usually advanced) cirrhosis.
- Abnormal elevation of liver enzymes in the blood (such as ALT and AST) that are obtained routinely as part of yearly health examinations suggests inflammation or injury to the liver from many causes as well as cirrhosis.
- Auto-antibodies (antinuclear antibody, anti-smooth muscle antibody and anti-mitochondrial antibody) can be detected in the blood and may be a clue to the presence of autoimmune hepatitis or primary biliary cirrhosis, both of which can lead to cirrhosis.
- Liver cancer (hepatocellular carcinoma) may be detected by CT and MRI scans or ultrasound of the abdomen. Liver cancer most commonly develops in individuals with underlying cirrhosis.
- If there is an accumulation of fluid in the abdomen, a sample of the fluid can be removed, examined and tested. The results of testing may suggest the presence of cirrhosis as the cause of the fluid.
Diagnosing hepatic encephalopathy2
The onset of HE often is insidious and is characterised by subtle and sometimes intermittent changes in memory, personality, concentration and reaction times. It is primarily a diagnosis of exclusion and so all other etiologies of altered mental status must be effectively ruled out.
Findings on physical examination in HE include asterixis and fetor hepaticus. An elevated arterial or free venous serum ammonia level is the classic laboratory abnormality reported in patients with HE. Electroencephalography may be helpful in the initial workup of a patient with cirrhosis and altered mental status, when ruling out seizure activity may be necessary. Computed tomography (CT) scanning and magnetic resonance imaging (MRI) studies of the brain may be important in ruling out intracranial lesions when the diagnosis of HE is in question.3 Classic EEG changes associated with HE are high-amplitude low-frequency waves and triphasic waves. However, these findings are not specific for HE.
Elevated blood ammonia in hepatic encephalopathy4
An elevated blood ammonia level is the classic laboratory abnormality reported in patients with HE.3 This finding may aid in correctly diagnosing patients with cirrhosis who present with altered mental status. Only arterial or free venous blood specimens must be assayed when checking the ammonia level. Blood drawn from an extremity to which a tourniquet has been applied may provide a falsely elevated ammonia level when analysed.
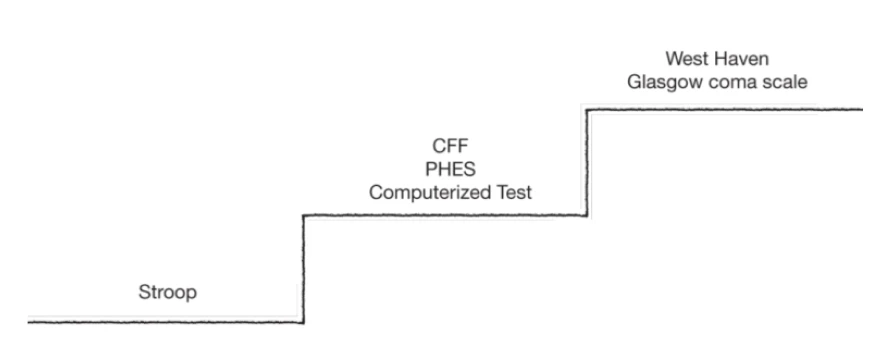
Deciphering the spectrum of low-grade HE in clinical practice – which tests to use when5
1. Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: part I. Diagnosis and evaluation. Am Fam Physician. 2006;74(5):756-62.
2. Heidelbaugh JJ, Sherbondy M. Cirrhosis and chronic liver failure: part II. Complications and treatment. Am Fam Physician. 2006;74(5):767-76.
3. Singhal A et al. Magnetic resonance T2-relaxometry and 2D L-correlated spectroscopy in patients with minimal hepatic encephalopathy. J Magn Reson Imaging. 2009;30(5):1034-41.
4. Stahl J. Studies of the blood ammonia in liver disease. Its diagnostic, prognostic, and therapeutic significance. Ann Intern Med. 1963;58:1-24.
5. Romero-Gómez M, Ampuero J. Deciphering the Spectrum of Low-Grade Hepatic Encephalopathy in Clinical Practice. Gastroenterology. 2014 Feb 21. [Epub ahead of print]